What is a pedriatric cardiologist?
A physician who after obtaining a basic medical degree completes a specialty in Pediatrics (diseases of children) and after that receives specialized training in diseases of the heart and circulatory system of children and adults with congenital heart disease.
Therefore, this specialist must have training in pediatrics and cardiology. In the area of pediatrics, he or she must know the medical afflictions and surgical interventions that are frequent in children such as chromosomal and hereditary diseases with which heart malformations are frequently found.
Therefore, this specialist must have training in pediatrics and cardiology. In the area of pediatrics, he or she must know the medical afflictions and surgical interventions that are frequent in children such as chromosomal and hereditary diseases with which heart malformations are frequently found.
What are congenital heart diseases?
Congenital heart diseases are anatomic abnormalities of one or more of the four heart chambers, the walls that separate them, the valves, the exit routes (ventricular zones where blood leaves the heart), or the vessels that leave or arrive at the heart.
Congenital heart diseases are not uncommon. Eight of every 1,000 children born, almost one of every one hundred, suffer this problem. The news that a child has a cardiac injury is always a source of great concern to the parents. Truly enough, if a congenital heart problem I not diagnosed sufficiently early and not treated adequately it may put in risk the life of the child, specially when the problem manifests itself during the first month after birth.
In older children the heart injury when left untreated may provoke a poor quality of life, or even shorten it.
However, at the present time the medical detection of congenital heart diseases happens during the first days, weeks or months after birth, in such a way that it is possible to plan the appropriate medical or surgical intervention to correct the problem. The great majority of congenital heart diseases may be corrected completely and definitively or almost definitely, allowing the child to live a normal or almost normal life.
There are more than 50 types of injuries or abnormalities. However, very frequently several of these combine themselves into several injuries in the same child. Many congenital diseases are really multiple injuries, such as the case of Tetralogy of Fallot. There is no direct relationship, however, between the number of associated lesions and the gravity of the case.
Congenital heart diseases are not uncommon. Eight of every 1,000 children born, almost one of every one hundred, suffer this problem. The news that a child has a cardiac injury is always a source of great concern to the parents. Truly enough, if a congenital heart problem I not diagnosed sufficiently early and not treated adequately it may put in risk the life of the child, specially when the problem manifests itself during the first month after birth.
In older children the heart injury when left untreated may provoke a poor quality of life, or even shorten it.
However, at the present time the medical detection of congenital heart diseases happens during the first days, weeks or months after birth, in such a way that it is possible to plan the appropriate medical or surgical intervention to correct the problem. The great majority of congenital heart diseases may be corrected completely and definitively or almost definitely, allowing the child to live a normal or almost normal life.
There are more than 50 types of injuries or abnormalities. However, very frequently several of these combine themselves into several injuries in the same child. Many congenital diseases are really multiple injuries, such as the case of Tetralogy of Fallot. There is no direct relationship, however, between the number of associated lesions and the gravity of the case.
What are the causes for congenital heart diseases?
The real causes for the majority of the abnormalities and deficiencies in the development of the heart are unknown, and so are the causes for congenital heart diseases. We may know them in the future.
At the present time we only know the risk factors or circumstances that favor having a child with heart disease:
One of the frequently asked questions that parents ask themselves is if it is worthwhile to take the risk of having another child. The answer is straightforward for the majority of cases: YES, because the risk of having another child with congenital heart disease, even though it may be slightly higher than for those couples without children with congenital heart disease, it is still very low.
It is nevertheless recommended to obtain the genetic advice or statistical calculation of the probability of having another child with congenital heart disease, which is calculated using multiple specific factors particular to the couple.
At the present time we only know the risk factors or circumstances that favor having a child with heart disease:
- Age of parents (younger than 18 or older than 35)
- Family history of congenital heart disease
- Children with chromosome alterations (Down syndrome, etc.)
- Mother factors related to diabetes, alcoholism, lupus, phenylketunoria and rubella during pregnancy
- Consuming drugs such as amphetamines, hydantoin, timetadiona, lithium and thalidomide during pregnancy
One of the frequently asked questions that parents ask themselves is if it is worthwhile to take the risk of having another child. The answer is straightforward for the majority of cases: YES, because the risk of having another child with congenital heart disease, even though it may be slightly higher than for those couples without children with congenital heart disease, it is still very low.
It is nevertheless recommended to obtain the genetic advice or statistical calculation of the probability of having another child with congenital heart disease, which is calculated using multiple specific factors particular to the couple.
What is a heart murmur?
A heart murmur is an acoustic phenomenon (sound or noise) that we can hear between the two normal heart sounds with the help of a stethoscope. A murmur is not necessarily a disease or something we can see or touch.
Normal heartbeat
Mitral Stenosis
Pulmonary Stenosis
Aortic Regurgitation
Mitral Regurgitation
A heart murmur may be normal (innocent) or pathological. The latter generally indicates the presence of a heart defect in one of its walls, valves or arteries. Therefore if the pediatrician detects a heart murmur and has doubts about it the child should be referred to a pediatric cardiologist.
Normal heartbeat
Mitral Stenosis
Pulmonary Stenosis
Aortic Regurgitation
Mitral Regurgitation
A heart murmur may be normal (innocent) or pathological. The latter generally indicates the presence of a heart defect in one of its walls, valves or arteries. Therefore if the pediatrician detects a heart murmur and has doubts about it the child should be referred to a pediatric cardiologist.
What is an innocent heart murmur?
An innocent or normal heart murmur is one that does not surpass the third degree. On certain occasions it is difficult to hear a heart murmur in a child when he is crying. Heart murmurs may appear at birth or after the age of two and they become more intense when there is anemia, fever, infections or excitation.
The murmur is caused by blood flowing inside the walls of blood vessels or by the vibration produced when blood strikes a very elastic heart that when it vibrates produces a particular sound.
To be certain of what kind of murmur it is, the pediatric cardiology specialist must evaluate the patient. The evaluation consists of carefully listening to the heart noises, check the patient’s pulses, and performing an EKG (allows us to evaluate the electrical activity of the heart). A chest X-ray gives us more information about the size of the heart and other valuable data.
In the case of an innocent heart murmur, the child’s heart is normal and will not present symptoms such as chest pain, difficulty to gain weight, and shortness of breathing. It will not be necessary to curtail his activities. He can play, run, exercise and travel. He does not need to be pampered nor does he require further visits to the doctor unless you or your doctor have remaining doubts.
The murmur is caused by blood flowing inside the walls of blood vessels or by the vibration produced when blood strikes a very elastic heart that when it vibrates produces a particular sound.
To be certain of what kind of murmur it is, the pediatric cardiology specialist must evaluate the patient. The evaluation consists of carefully listening to the heart noises, check the patient’s pulses, and performing an EKG (allows us to evaluate the electrical activity of the heart). A chest X-ray gives us more information about the size of the heart and other valuable data.
In the case of an innocent heart murmur, the child’s heart is normal and will not present symptoms such as chest pain, difficulty to gain weight, and shortness of breathing. It will not be necessary to curtail his activities. He can play, run, exercise and travel. He does not need to be pampered nor does he require further visits to the doctor unless you or your doctor have remaining doubts.
When should I suspect the presence of heart disease?
You should notice certain symptoms that could indicate the need to seek medical attention. If your child seem to be having problems breathing call your pediatrician immediately. Other signs that require immediate medical attention are the following:
- Bluish skin around the mouth or lips and tongue (cyanosis).
- Heavy breathing or difficulty breathing, look fatigued.
- Loss of appetite or difficulty eating (which may be associated with the change in color).
- Excessive sweating when eating.
- Delays in growing (the child does not gain weight or loses weight).
- Decrease in the level of energy or activity.
- Inexplicable long-lasting fever.
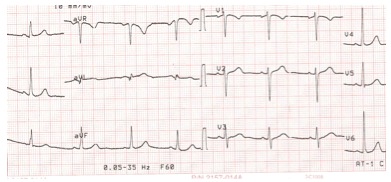
What is an electrocardiogram?
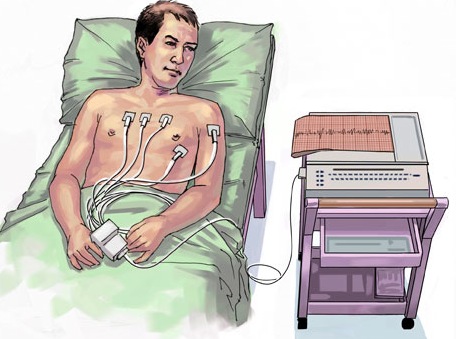
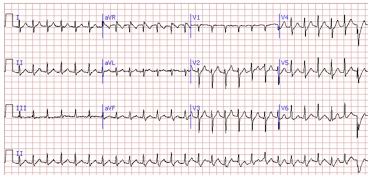
"ECG", "EKG" or "electrocardiogram" all refer to the same test, which is a simple and painless test that records the changes in the electrical activity of the heart on graph paper.
An electrocardiogram helps identify heart rhythm abnormalities (arrhythmias) and imbalances of the salts of the body. It can also provide information about the size or thickness of the heart chambers and the relative position of the heart in the chest.
Does an electrocardiogram / EKG hurt?
No, an electrocardiogram is painless. In fact, the most painful part of the process is removing the electrodes which are less sticky than even adhesive bandages.
How is it done?
A technician or nurse will take the patient into a room and have the patient take off his / her shirt and lie down on an examination table or bed. Twelve stickers called electrodes are attached to the chest, shoulders and each leg. A wire will then be attached to each electrode. After the patient is very still and relaxed, the technician will press a button on the electrocardiogram machine and the recording will be done. The recording generally takes less than a minute.
Are there any risks involved when getting an EKG?
The only risk to the test is a skin allergy to the adhesive of the electrodes that may result in temporary redness and irritation of the skin where the electrodes are applied.
An electrocardiogram helps identify heart rhythm abnormalities (arrhythmias) and imbalances of the salts of the body. It can also provide information about the size or thickness of the heart chambers and the relative position of the heart in the chest.
Does an electrocardiogram / EKG hurt?
No, an electrocardiogram is painless. In fact, the most painful part of the process is removing the electrodes which are less sticky than even adhesive bandages.
How is it done?
A technician or nurse will take the patient into a room and have the patient take off his / her shirt and lie down on an examination table or bed. Twelve stickers called electrodes are attached to the chest, shoulders and each leg. A wire will then be attached to each electrode. After the patient is very still and relaxed, the technician will press a button on the electrocardiogram machine and the recording will be done. The recording generally takes less than a minute.
Are there any risks involved when getting an EKG?
The only risk to the test is a skin allergy to the adhesive of the electrodes that may result in temporary redness and irritation of the skin where the electrodes are applied.
What is an echocardiogram?
An echocardiogram is similar to a sonogram many women have had before a child was born; however, the echocardiogram focuses specifically on the heart and blood vessels around the heart.
An echocardiogram ("echo") is an ultrasound test that uses high frequency sound waves (non-radioactive) for viewing the heart. It is a safe and painless procedure that helps doctors diagnose heart problems.
Pictures of the child's heart can be viewed on a small monitor while the procedure is being performed. It is a non-invasive test (no probes or needles) and everything is done from the outside of the body.
It is a painless test that does not produce secondary effects. Thanks to this test we can find out many details about the functioning of the heart.
An echocardiogram ("echo") is an ultrasound test that uses high frequency sound waves (non-radioactive) for viewing the heart. It is a safe and painless procedure that helps doctors diagnose heart problems.
Pictures of the child's heart can be viewed on a small monitor while the procedure is being performed. It is a non-invasive test (no probes or needles) and everything is done from the outside of the body.
It is a painless test that does not produce secondary effects. Thanks to this test we can find out many details about the functioning of the heart.
What is a fetal echocardiogram?
A pediatric cardiologist performs the fetal echocardiogram. The test may be carried out using abdominal or transvaginal ultrasound.
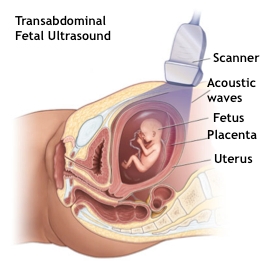

During the exam, the transducer probe is moved to obtain images of different areas and structures of the fetal heart. Some of the techniques often used to obtain detailed information of the fetus heart include the following:
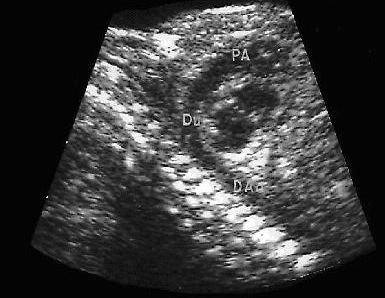
Fetal echocardiography can help detect heart abnormalities before birth allowing for a faster medical or surgical intervention once the baby is born. This increases the probability of survival of babies with severe cardiac defects after delivery.
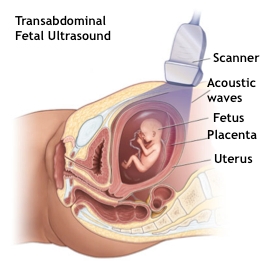
- Abdominal ultrasound. Gel is applied in the abdomen and a an ultrasound transducer slides over the gel to create the image.
- Transvaginal ultraosund. A small ultrasound transducer is inserted in the vagina and placed over its front side to create the images. Transvaginal ultrasound produces better images than abdominal ultrasound and it is therefore used during early pregnancy.

During the exam, the transducer probe is moved to obtain images of different areas and structures of the fetal heart. Some of the techniques often used to obtain detailed information of the fetus heart include the following:
- 2-D Echocardiography (bi-dimensional). This technique is used to observe the real structures of the heart and their motion. The image of the 2-D ultrasound appears in the monitor n the shape of a cone where one can observe the structures of the heart in real time. This allows the doctor to see the various heart structures in operation to evaluate them.
- Doppler Echocardiography. Is used to measure and evaluate the flow of blood through the chambers and valves of the heart. The amount of blood that pumps with every heartbeat is an indication of the functioning of the heart. Also, the Doppler eco can detect abnormal blood flow inside the heart, which would indicate problems such as an opening between the chambers, the incorrect functioning of any of the four cardiac valves, or a deterioration of the walls that separate the chambers.
- Doppler in Color. It is an improved version of Doppler echocardiography. In Doppler in color different colors indicate the direction of blood flow. This simplifies the interpretation of the images.
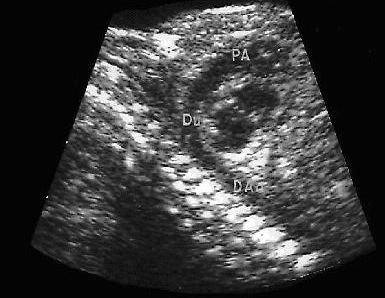
Fetal echocardiography can help detect heart abnormalities before birth allowing for a faster medical or surgical intervention once the baby is born. This increases the probability of survival of babies with severe cardiac defects after delivery.
What is a Holter Monitor?
A Holter monitor is a 24-hour recording of the electrical activity of the heart. The monitor is a diagnostic tool used to record the rate and rhythm of the heart. Irregularities such as fast heart rate (tachycardia) slow heart rate (bradycardia), and abnormal rhythms of the heart can be recorded.
Because many irregularities in heart rate or rhythm may not be present all of the time, a standard electrocardiogram (EKG) may miss them.
By recording the heart rate and rhythm continuously for 24 hours throughout the various activity levels a child goes through, there is a greater chance of detecting abnormalities.

How Holter monitoring is performed
The recorder is applied to the patient by an experienced technician. The technician attaches five electrode patches (with wires) to the child's chest. The electrodes are like conventional EKG patches and make it possible to record the heart's electrical activity. The wires are attached to a tape recorder that is worn for 24 hours on a belt around the waist or on a shoulder strap like a shoulder bag.
The patient or parents can remove the monitor after 24 hours or bring the child back to Cincinnati Children's Heart Institute for removal of the monitor. If the parent removes the monitor, it should be brought back to the Heart Institute or shipped back via overnight delivery within 24 hours so the tracing can be analyzed.
A patient or parent should keep a log of activities during the day that the monitor is attached, especially recording any symptoms that develop that are suspected of being related to a cardiac rhythm problem.
Is a Holter Monitor uncomfortable or painful?
The Holter Monitor test can be a bit uncomfortable for some patients, as the electrodes and tape can irritate the skin, but it is not painful.
Is there any preparation needed for a Holter Monitor?
There is no prior preparation for the test. If other tests are scheduled that day the Holter monitor must be the last test performed, as it has to be on for 24 hours. The child may not bathe with the monitor or get it wet.
Because many irregularities in heart rate or rhythm may not be present all of the time, a standard electrocardiogram (EKG) may miss them.
By recording the heart rate and rhythm continuously for 24 hours throughout the various activity levels a child goes through, there is a greater chance of detecting abnormalities.

How Holter monitoring is performed
The recorder is applied to the patient by an experienced technician. The technician attaches five electrode patches (with wires) to the child's chest. The electrodes are like conventional EKG patches and make it possible to record the heart's electrical activity. The wires are attached to a tape recorder that is worn for 24 hours on a belt around the waist or on a shoulder strap like a shoulder bag.
The patient or parents can remove the monitor after 24 hours or bring the child back to Cincinnati Children's Heart Institute for removal of the monitor. If the parent removes the monitor, it should be brought back to the Heart Institute or shipped back via overnight delivery within 24 hours so the tracing can be analyzed.
A patient or parent should keep a log of activities during the day that the monitor is attached, especially recording any symptoms that develop that are suspected of being related to a cardiac rhythm problem.
Is a Holter Monitor uncomfortable or painful?
The Holter Monitor test can be a bit uncomfortable for some patients, as the electrodes and tape can irritate the skin, but it is not painful.
Is there any preparation needed for a Holter Monitor?
There is no prior preparation for the test. If other tests are scheduled that day the Holter monitor must be the last test performed, as it has to be on for 24 hours. The child may not bathe with the monitor or get it wet.
What is excercise testing?
The exercise test is a valuable tool for gaining information about a child's heart and heart functioning, and their aerobic fitness. Most tests of the heart are done with a person at rest, but most of the time people are active. Exercise testing can give information about how the heart responds to the extra demands of activity.
The graded exercise test collects information that is key for defining how a child's heart responds to various levels of exercise and assesses their level of fitness.

What the exercise test entails
Based on the individual's needs, age or ability, the exercise may be carried out on a treadmill.The test consists of progressive stages that vary in speed and elevation. The child will have a blood pressure cuff on their right arm. This will be inflated periodically to measure blood pressure at various levels of the exercise test.
To monitor the heart, an electrocardiogram (EKG) consisting of 10 electrodes attached to the child's chest and torso is used.
Is the exercise test painful or uncomfortable?
The exercise test may be uncomfortable for the patient's legs, as the tests progress through the stages. The patient's legs may start to feel tired and the child will start to breathe more heavily during the progression of the exercise test.
Is the exercise test risky or dangerous?
The exercise test is not risky or dangerous. Complications rarely occur, and if they do, the staff is equipped and trained to handle those rare occasions.
Because the heart's function is being constantly monitored during the test, the exercise will be stopped if anything worrisome is observed.
No one is pushed to exercise at a level beyond what they are comfortable with. If a child becomes too tired or experiences chest pain or dizziness, the exercise is stopped.
Are there any special preparations before or after the exercise test?
The child must not intake any caffeine that day and should not eat for two hours before the test. The child should come prepared to do exercise in comfortable clothing and sneakers.
Who performs the exercise test?
Experienced exercise technicians administer the test under the supervision of a physician.
Who interprets the exercise test?
A pediatric cardiologist interprets the exercise test.
The graded exercise test collects information that is key for defining how a child's heart responds to various levels of exercise and assesses their level of fitness.

What the exercise test entails
Based on the individual's needs, age or ability, the exercise may be carried out on a treadmill.The test consists of progressive stages that vary in speed and elevation. The child will have a blood pressure cuff on their right arm. This will be inflated periodically to measure blood pressure at various levels of the exercise test.
To monitor the heart, an electrocardiogram (EKG) consisting of 10 electrodes attached to the child's chest and torso is used.
Is the exercise test painful or uncomfortable?
The exercise test may be uncomfortable for the patient's legs, as the tests progress through the stages. The patient's legs may start to feel tired and the child will start to breathe more heavily during the progression of the exercise test.
Is the exercise test risky or dangerous?
The exercise test is not risky or dangerous. Complications rarely occur, and if they do, the staff is equipped and trained to handle those rare occasions.
Because the heart's function is being constantly monitored during the test, the exercise will be stopped if anything worrisome is observed.
No one is pushed to exercise at a level beyond what they are comfortable with. If a child becomes too tired or experiences chest pain or dizziness, the exercise is stopped.
Are there any special preparations before or after the exercise test?
The child must not intake any caffeine that day and should not eat for two hours before the test. The child should come prepared to do exercise in comfortable clothing and sneakers.
Who performs the exercise test?
Experienced exercise technicians administer the test under the supervision of a physician.
Who interprets the exercise test?
A pediatric cardiologist interprets the exercise test.
What is ABPM (Ambulatory Blood Pressure Monitoring)?
It’s a support technique that allows us to take serial measurements of blood pressure (BP) during a certain period of time (typically 24 hours), performed in an ambulatory manner, by means of placing a sphygmomanometer connected to a recorder that automatically performs the measurements, which are later on analyzed by the physician. This allows us to observe variations on blood pressure during the day, determine if the patient experiences White Coat Hypertension, evaluate the response to medication for controlling BP, etc.
White Coat Hypertension is what happens with certain persons with normal blood pressure who suffer a transient elevation of blood pressure when it’s measured by a doctor or nurse. It is important to know this phenomenon to avoid making the wrong diagnosis on patients who have normal blood pressure throughout the day. To make this observation blood pressure is measured in their day-to-day environment.
Frequently these patients also experience a rise in blood pressure in the presence of abnormal and typically stressful situations , such as hurries, public appearances, when they feel strong emotions, and so on.
Because of this reason the patient must be observed with a certain frequency and, even when not a candidate for treatment with medication, he must follow certain preventive measures and periodic blood pressure control.
White Coat Hypertension is what happens with certain persons with normal blood pressure who suffer a transient elevation of blood pressure when it’s measured by a doctor or nurse. It is important to know this phenomenon to avoid making the wrong diagnosis on patients who have normal blood pressure throughout the day. To make this observation blood pressure is measured in their day-to-day environment.
Frequently these patients also experience a rise in blood pressure in the presence of abnormal and typically stressful situations , such as hurries, public appearances, when they feel strong emotions, and so on.
Because of this reason the patient must be observed with a certain frequency and, even when not a candidate for treatment with medication, he must follow certain preventive measures and periodic blood pressure control.
What is arrhythmia?
What is an arrhythmia?
An arrhythmia (also called a dysrhythmia), is an abnormal rhythm of the heart that makes it pump inefficiently.
Arrhythmias mac cause problems in the contractions of the heart chambers due to:
- Not allowing the ventricles (lower chambers) to fill with an adequate amount of blood because the electrical signal makes the heart beat too fast.
- Not allowing the heart to pump enough blood to the body because the electrical signal makes the heart beat too slow or irregularly.
¿What are the symptoms of arrhythmia?
The following is a list of the most common symptoms of arrhythmia. However, each child may experience them in a different form. The symptoms may include?
▪ Weakness
▪ Fatigue
▪ Palpitations
▪ Low blood pressure
▪ Dizziness
▪ Fainting spells
▪ Paleness
▪ Loss of appetite
The symptoms of arrhythmia can be similar to the ones of other cardiac problems or diseases. Always consult your doctor to get a diagnosis.
Another indication that an arrhythmia exists is a change in the pattern of an electrocardiogram (EKG). However, changes in the EKG are only seen when the test is performed under medical supervision in a hospital or other medical institution. Because the symptoms mentioned earlier may indicate the presence of an arrhythmia, it is common to request an EKG to children that experience them.
My child fainted. What should I do?
You should talk to your primary care provider as soon as possible.
The episode of loss of consciousness and fall is called a syncope or lipothymy. The most commonly observed in children and adolescents is the vasovagal syncope in situations involving fasting, closed environments, too much time standing up, stress, fear, etc.
Usually the child perceives that something is wrong. He becomes restless, may have a headache and be nauseous. He can also be irritable, pale of skin, with hands and feet cold. All these symptoms indicate that the child will faint and fall.
The duration of these episodes is short and recuperation is complete within a few minutes. Very frequently similar incidents occur in close relatives. It is also associated with family backgrounds that include migraines and weeping spasms.
It is recommended to study the child to discard other mainly cardiac diseases such as arrhythmias or structural cardiopathies (alterations of the heart’s anatomy), for which the patient will be referred to a pediatric cardiologist. Other alterations are neurological such as convulsions that cause loss of consciousness and abrupt fall but with marked confusion and drowsiness after the event without being able to remember what happened.
The child must be evaluated by a pediatrician who after an interrogation and physical exam may, depending on the findings, request an electrocardiogram and blood tests to discard anemia or glucose changes, etc. If fainting reoccurs or there are doubts in the diagnosis, a neurological evaluation may be requested to discard convulsion episodes.
There is study called Tilt Test that investigates the relationship between changes in blood pressure in different body positions (laying down, sitting or standing up). The study is performed using special equipment consisting of a mobile stretcher and blood pressure sensors that are attached to the patient. The study is performed gradually and under careful professional supervision.
The treatment of fainting spells consists first of preventing them by avoiding long hours without food intake, prolonged periods of time standing up or in enclosed environments, etc. At the moment when starting symptoms appear (paleness, dizziness, nausea, etc.), the patient should sit down or lie down with legs elevated to improve blood circulations.
With certain specific cases of syncope, the specialist will determine the need for special medication.
The episode of loss of consciousness and fall is called a syncope or lipothymy. The most commonly observed in children and adolescents is the vasovagal syncope in situations involving fasting, closed environments, too much time standing up, stress, fear, etc.
Usually the child perceives that something is wrong. He becomes restless, may have a headache and be nauseous. He can also be irritable, pale of skin, with hands and feet cold. All these symptoms indicate that the child will faint and fall.
The duration of these episodes is short and recuperation is complete within a few minutes. Very frequently similar incidents occur in close relatives. It is also associated with family backgrounds that include migraines and weeping spasms.
It is recommended to study the child to discard other mainly cardiac diseases such as arrhythmias or structural cardiopathies (alterations of the heart’s anatomy), for which the patient will be referred to a pediatric cardiologist. Other alterations are neurological such as convulsions that cause loss of consciousness and abrupt fall but with marked confusion and drowsiness after the event without being able to remember what happened.
The child must be evaluated by a pediatrician who after an interrogation and physical exam may, depending on the findings, request an electrocardiogram and blood tests to discard anemia or glucose changes, etc. If fainting reoccurs or there are doubts in the diagnosis, a neurological evaluation may be requested to discard convulsion episodes.
There is study called Tilt Test that investigates the relationship between changes in blood pressure in different body positions (laying down, sitting or standing up). The study is performed using special equipment consisting of a mobile stretcher and blood pressure sensors that are attached to the patient. The study is performed gradually and under careful professional supervision.
The treatment of fainting spells consists first of preventing them by avoiding long hours without food intake, prolonged periods of time standing up or in enclosed environments, etc. At the moment when starting symptoms appear (paleness, dizziness, nausea, etc.), the patient should sit down or lie down with legs elevated to improve blood circulations.
With certain specific cases of syncope, the specialist will determine the need for special medication.